Medicaid Reform
The Federal Medicaid Act was enacted in 1965 as part of the broader Social Security Act.
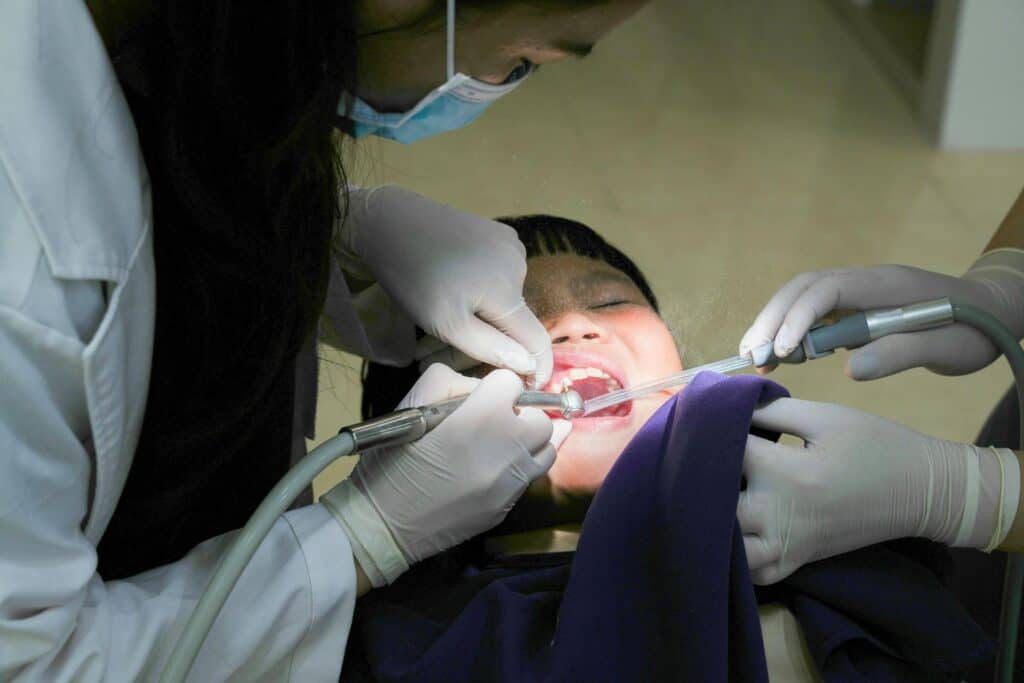
The primary aim of Medicaid is to ensure that low-income populations have access to necessary medical services, which includes dental care.
Under the Medicaid Act, the federal government provides approximately 50% of funding to states in return for states FULLY complying with the Medicaid Act. While states have flexibility in determining the specific benefits, eligibility criteria, and administration of their Medicaid programs, the states may not fail to cover any service that is “medically necessary” – a term that also encompasses dental needs.
Children’s Medicaid coverage (known as EPSDT -Early Periodic Screening, Diagnostic, and Treatment), is highly regulated by the Medicaid Act language. State Medicaid programs must cover ALL medically necessary needs for children under 21 years of age in order to receive any federal funds. Adult Medicaid coverage is optional for states.
The Federal government monitors state plan compliance with the Medicaid Act using the Center for Medicare and Medicaid Services (CMS).
But are the states living up to their DENTAL obligations in the Medicaid Act, and is CMS doing a good job enforcing the Medicaid Act?
The answer is a resounding “No” – in FIVE ways.
The AADIQ wants to remedy these state government violations of the Medicaid Act and ensure that CMS does its duty, as prescribed by law.
1. GEOGRAPHIC AREA REQUIREMENT
Under 42USC-1396a(30)(A), states must provide “Payment Sufficient to enlist enough providers so that care and services are available under the plan at least to the extent that such care and services are available to the general population in the geographic area.”
States are out of compliance because they do not even compare the availability of “CARE AND SERVICES” to the “GENERAL POPULATION” in the geographic area.

2. MAINTENANCE OF DENTAL HEALTH REQUIREMENT
42USC-1396d(r)(3) states “Which shall at a minimum include relief of pain and infections, restoration of teeth, and maintenance of dental health.”
Most states are out of compliance because they deny treatments that the professional standard of care qualifies as necessary for dental health maintenance.
3. NECESSARY CARE NOT COVERED BY STATE PLAN REQUIREMENT
Under 42USC-1396d(r)(5) “Such other necessary health care, diagnostic services, treatment, and other measures described in subsection (a) of this section to correct or ameliorate defects and physical and mental illnesses and conditions discovered by the screening services, whether or not such services are covered under the State plan.”
States are out of compliance because officers are trained to believe that they must follow the state plan’s limitations. They are not trained to make exceptions as the Federal Medicaid Act language above requires. (eg. a patient that lost a crown must get another crown, regardless of time limitations).


4. REASONABLE PROMPTNESS REQUIREMENT
42USC-1396a(a)(8) states: “Provide that all individuals wishing to make application for medical assistance under the plan shall have the opportunity to do so, and that such assistance shall be furnished with reasonable promptness to all eligible individuals.”
Most states are out of compliance because their dental insurance contractors systematically take too long to make determinations on care.
5. COMPARABILITY REQUIREMENT: “Diagnosis Discrimination”
Under 42CFR-440.230(c) “The Medicaid agency may not arbitrarily deny or reduce the amount, duration, or scope of a required service under 440.210 and 440.220 to an otherwise eligible beneficiary solely because of the diagnosis, type of illness, or condition.”
Under 42USC-1396a(a)(10)(B)(i) “Medical assistance made available to any individual…shall not be less in amount, duration, or scope than the medical assistance made available to any other such individual.”
Jacobus vs Dept of Path – 2004 Vt
“Therefore the state must also cover preventative orthodontic treatment where it is of equal or greater severity as conditions covered by the State’s criteria.
Most states are out of compliance because they structure their authorizations to discriminate against comparable conditions.

